TINY Elizabeth-May Woodsford was born 16 weeks early weighing just 1.5lb, after her mum’s very difficult pregnancy which saw her spend the last month in and out of hospital and have five blood transfusions.
Nicole Wilderspin, 27, who lives in Cross Keys with partner Andrew Woodsford, 30, said: “The pregnancy was very difficult. I was exhausted, extremely sick, and in a lot of pain from the start – belly pain and back pain and constant headaches.
“At around 10 weeks I had a massive bleed and pain to the point where I couldn’t even get up off the sofa.
“I was told my hormone levels where high and was not offered a scan, so we booked a private one. We were told the baby was fine. I was in shock but so happy everything seemed fine.
“Our normal 12-week scan showed what only could be explained as a second failed pregnancy sac. We were devastated but we still carried on and were advised to expect more bleeding. I had no more bleeding until 16 weeks, when I was told I had a low lying placenta and that I should try to relax.”
READ MORE:
- Wales 'will follow own path out of Covid restrictions'
- George Cross awarded to NHS Wales for pandemic response
- Pontypool Park 'thank you' for NHS and other key workers
At 18 weeks Ms Wilderspin fell down the stairs but was told it was nothing to worry about and the baby would be well protected.
She said: “Then the nightmare really began. Within four days of having my 19 weeks scan where we were told everything seemed fine, I began to bleed heavily. It was the start of May and my first admission to the Grange University Hospital was on May 3.
“I spent the whole month in and out of hospital with the advice of complete bed rest. I would be fine for a day or two, then the bleeding would get extremely heavy and I’d have to return. The staff were lovely but never confirmed the exact reason for my bleed. We were only ever told it was a low lying placenta and this happens.”
She was later diagnosed with placenta previa.
On May 25 she was back in hospital after being allowed home the day before.
“I had returned with extremely large blood clotting, bleeds and pain. They said I would very likely have my baby prematurely.
“I was put on a magnesium sulphate drip to help with the baby’s brain development and to slow down my body. I was given this three more times during the week, along with steroid injections.”
On May 30 it was decided it was time for Elizabeth-May to be born.
Ms Wilderspin, who works in the claims department at Admiral, said: “I had a normal delivery surprisingly and Elizabeth-May arrived on May 31. It was confirmed the clots I was losing had been parts of my placenta. It was all really frightening.”
Mr Woodsford, an aluminium fabricator, said: “It was very emotional. As I arrived in the room Nicole was in the middle of having an epidural. A doctor explained everything that was going on. It was quite a scary moment for me to digest as the odds of survival were stacked against Elizabeth-May.
“When she was delivered it was very stressful to watch because there were about 10 different doctors in the room. We didn’t get to see her for about 15 minutes and then the doctor came over and told us that she was stable, which was a huge relief and very emotional.”
Ms Wilderspin had lost more than 2,000ml of blood in the week before Elizabeth-May was born and had to have five blood transfusions, including two after her baby was born.
“The thought of having such a tiny baby at 24 weeks and one day, I can’t describe the feeling. The doctors were amazing and really supportive of both me and my partner.”
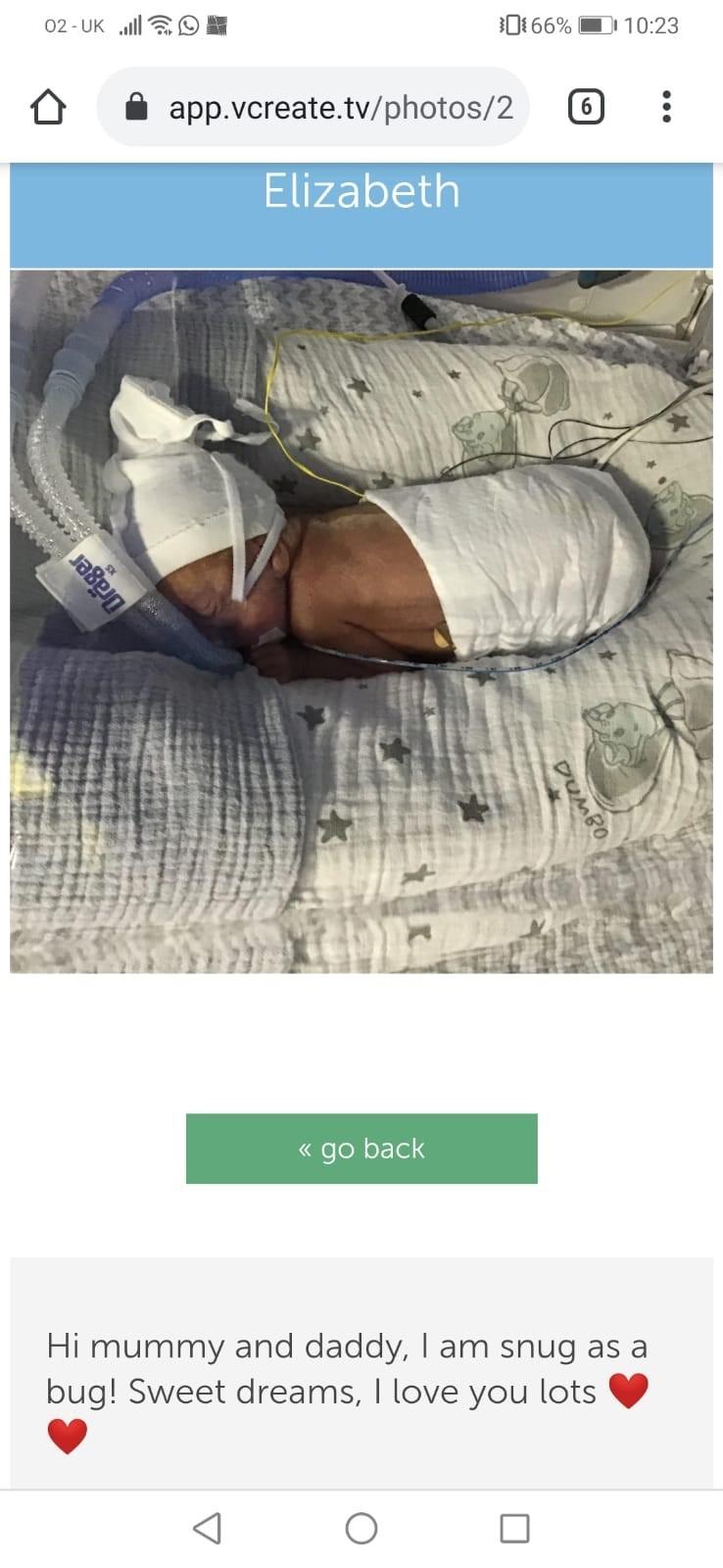
“She has been coping better than any of us expected. There are still massive hurdles for us to get through. She is so little and has to have such a long stay in the NICU (neonatal intensive care unit).
Nicole said: “This is something you never think about or think will happen to you. It’s very stressful, upsetting, and extremely difficult to juggle because we have two other small children.
“It is not nice seeing your child fighting everyday with wires all over her and her so tiny.
“There have been lots of tears so far, but worth it. We had to wait 12 days to be able to hug our little angel but when we did the happiness blew us away. When Elizabeth is stable we are always able to have cuddles.”
Nicole said: “Elizabeth still has a long way to go before she can come home. We have to take it day by day as she has good days and bad days. We are hopeful and thankful to have gotten this far.”
“Our family have been extremely supportive and have been a massive help having our girls to enable both of us to visit the baby together. We can’t thank them enough for everything they have done and they are all are excited to finally meet her.”
She said: “We would both like to say a massive thank-you to the staff at the Grange for everything they are doing to help baby Elizabeth-May and helping us to understand everything. Not only are they medical staff but they are like teachers showing us how to feed her through a tube and change her nappies and bedding (which is quite difficult to do in an incubator).”
















Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel